Targeting damaged cells may improve lung and ovarian cancer treatment
New research published today in Nature Aging by scientists at the University of Cambridge sheds light on why some lung and ovarian cancers stop responding to chemotherapy, and how this resistance might one day be prevented.
Platinum-based chemotherapy is commonly used to treat non-small cell lung cancer (NSCLC) and high-grade serous ovarian cancer (HGSOC). However, these treatments often don’t work as well as hoped for patients in the long term.
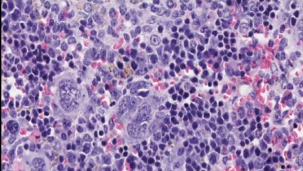
Research suggests that chemotherapy can lead to an increase in damaged cells that are ‘paused’, also called senescent cells, meaning that the cells are alive in the body but unable to grow or divide.
These senescent cells were once thought to help suppress cancer because they stop dividing. However, growing evidence now shows that over time they release chemical signals that encourage tumours to grow.
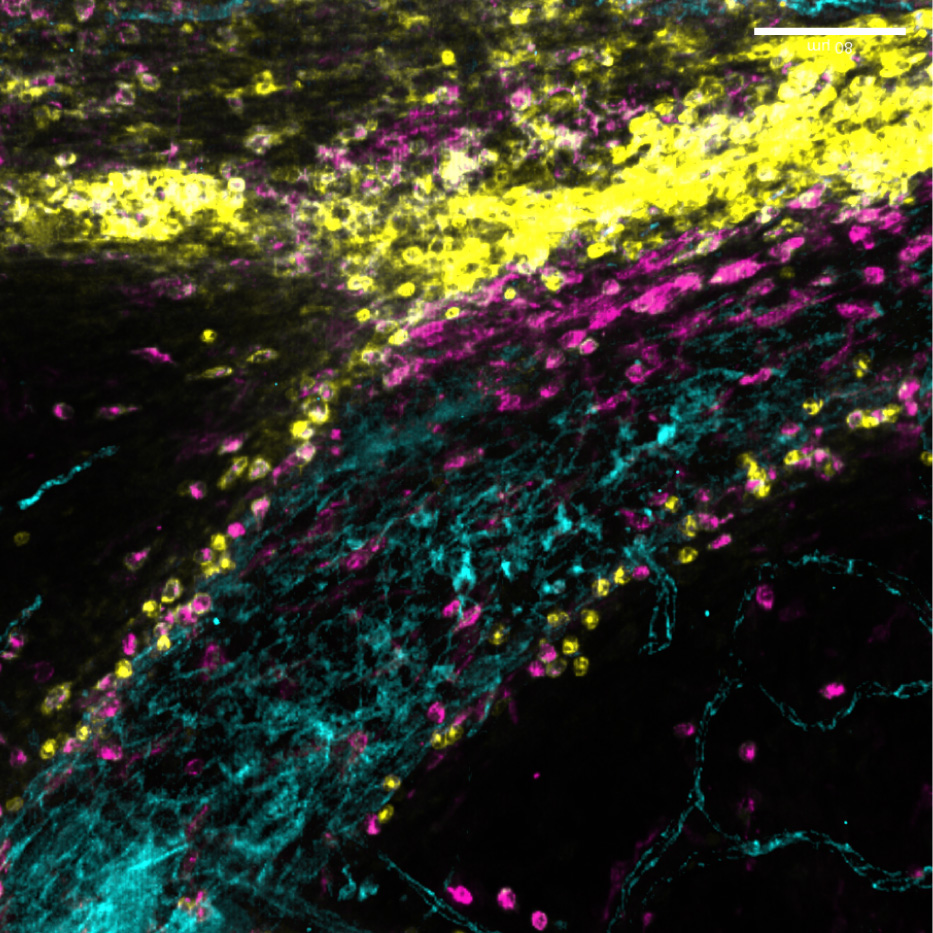
Working together, scientists from the Muñoz-Espín laboratory at the Early Cancer Institute and the Brenton and Narita groups at the Cancer Research UK Cambridge Institute investigated whether targeting senescent cells could help doctors tailor treatment for patients and prevent tumours from becoming resistant to chemotherapy.
Led by co-first authors Dr Estela Gonzalez-Gualda and Dr Marika Reinius, the team used mouse models and patient tumour samples to show that the anti-cancer medicines cisplatin and carboplatin, which are commonly used chemotherapy treatments, can push some cancer cells into this ‘paused’ senescent state.
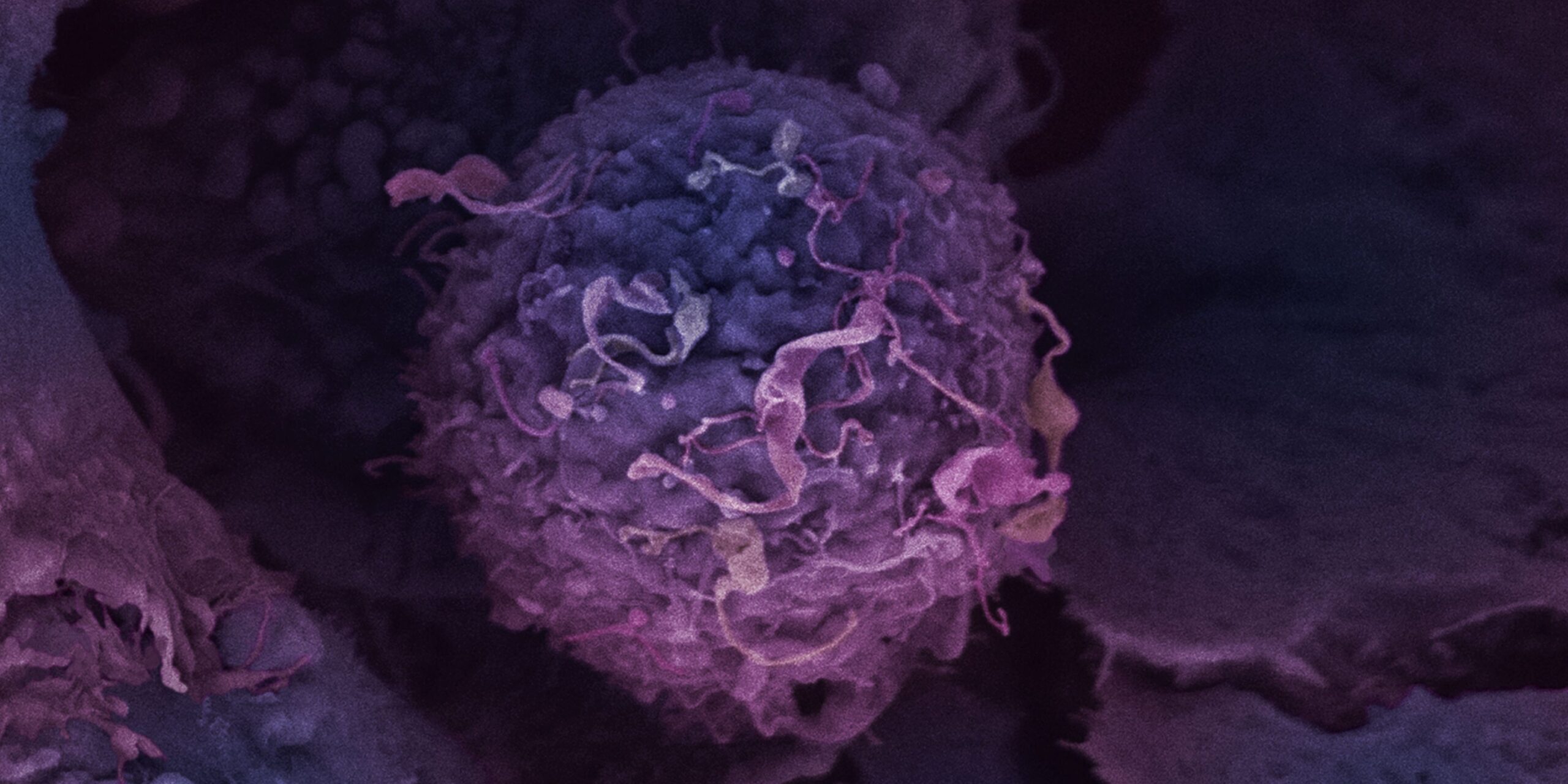
These senescent cells release high levels of a signalling molecule called TGFβ, which helps nearby cancer cells survive, grow, and resist treatment in both the lung and ovarian cancer models.
This effect was shown to be specific to platinum-containing chemotherapy. Other commonly used cancer drugs, such as docetaxel or palbociclib, did not trigger the same tumour-promoting response.
In several lung cancer models, the cisplatin-induced senescent cells were linked to faster tumour growth. Patient data, in collaboration with Prof Robert Rintoul (NHS Royal Papworth Hospital, also supports these findings, as people with non-small cell lung cancer whose tumours showed signs of senescence after platinum treatment had significantly worse outcomes. Similar effects also occurred in patients with ovarian cancer.
Age was also found to play an important role in treatment response. In mouse models, cisplatin chemotherapy created a lung environment in middle-aged animals that allowed tumours to grow more readily than in younger mice. This supports the idea that ageing and chemotherapy damage together creates conditions that help cancer develop.
Encouragingly, blocking the TGFβ signalling from the senescent cells, or removing senescent cells using drugs called senolytic agents, reduced tumour growth and improved survival rates in several lung cancer models.
This research suggests that pairing platinum chemotherapy with drugs that target senescent cells or TGFβ signalling could make treatment for patients more effective and help prevent resistance and cancer reoccurrence.
Prof Daniel Muñoz-Espín, Early Cancer Institute, said: “Previous reports in other cancer models provided evidence that the induction of senescence in response to chemotherapy can be tumour-promoting. However, the responsible protumorigenic factors and signals released from senescent cells were unknown.
It was very exciting to find that, among hundreds of proteins secreted by senescent cells, TGFβ ligands are key drivers of cancer progression and relapse. We also found that TGFβ signalling activates AKT/mTOR, a pathway that strongly promotes tumour growth.
The identification of this novel mechanism of chemotherapy resistance allowed us to prioritise precision medicine drugs to improve the therapeutic outcomes.”
Prof Masashi Narita, Cancer Research UK Cambridge Institute, said: “Cellular senescence has been extensively studied in normal cells, yet its occurrence and clinical relevance in cancer have remained unclear. This study refines the importance of therapy-induced senescence in cancers, revealing it as an active and targetable driver of tumour progression.”
“Carboplatin is a vital treatment for ovarian cancer patients and these exciting findings will now lead to trials adding senolytic medicines to chemotherapy to test whether we can remove harmful senescent cancer cells and improve outcomes.”
Prof James Brenton, Cancer Research UK Cambridge Institute
Related News
See all news-
New immune pathway offers treatment hope for childhood brain tumours
3rd February 2026
A newly discovered immune pathway could lead to gentler treatments for multiple childhood brain cancers, according to new research from our Gilbertson Group published today in Nature Genetics.
Find out more -
Hot flush treatment has anti-breast cancer activity, study finds
5th January 2026
A drug mimicking the hormone progesterone has anti-cancer activity when used together with conventional anti-oestrogen treatment for women with breast cancer, a new Cambridge-led trial has found.
Find out more -
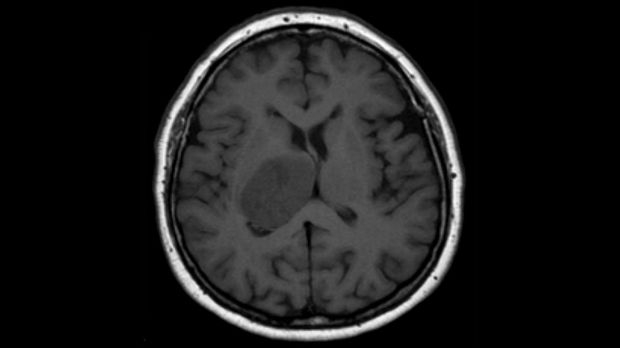
Dr Richard Mair to co-lead £13.7M investment for brain tumour research
19th December 2025
The National Institute for Health and Care Research (NIHR) has today announced a £13.7 million investment that will support ground-breaking research to develop novel brain tumour treatments in the UK.
Find out more